Antenatal Care
Antenatal Care
We delight in being able to provide care during this special time. All of our GPs are obstetric shared care providers in South Australia and therefore are able to provide care during your pregnancy in conjunction with major birthing units. Additionally, Dr Andrew provides intrapartum care at Mount Barker Hospital on a rostered basis. Dr Smith and Dr Andrew both hold advanced diplomas in Obstetrics and are able to manage more complex antenatal care.
Antenatal Appointment Schedule
We understand that this time can be overwhelming and confusing! To help make things a bit clearer, we have created an Antenatal Appointment Schedule which details what your appointments will look like when you come to us for GP Shared Care. In this document we outline how often you will need antenatal checks, what routine blood tests are usually requested, and lots more. We hope this helps!
To view this schedule, click here.
Early Pregnancy Wellbeing
For our early pregnancy services, please visit our Early Pregnancy Wellbeing page. These services are available to everyone, whether you are an antenatal patient of ours or if you are receiving pregnancy care elsewhere.
On this page you will see information regarding early pregnancy bleeding, reassurance services (i.e. early pregnancy ultrasound) and nausea and vomiting (hyperemesis) management.
You can fill out a form to request an appointment or call back from a clinical staff member on this page.
Gestational Diabetes
All pregnant women should be screened for gestational diabetes at around 26-28 weeks, and those with risk factors may need to be screened at 14-16 weeks too. Unfortunately, the test can be a little unpleasant – it involves fasting, having 3 sets of bloods taken over 2 hours, and drinking a very sweet, mildly fizzy drink. However, it is a very important test as many women who get diagnosed with gestational diabetes have no, or very few, risk factors for it. Importantly, it is nothing that YOU have done to cause this condition. It is entirely due to your placenta and your genetic predisposition to Type 2 diabetes. To reiterate: you cannot cause gestational diabetes by eating too much sugar.
If you are diagnosed with gestational diabetes, there are many things you can do to make sure your pregnancy continues to be healthy. You will be referred to see a diabetes nurse educator and dietician. The diabetes nurse educator will give you a glucometer, which is how you will measure your blood sugar levels. This will need to be done 4 times a day initially: fasting in the morning and then 2 hours after the start of each main meal. The results need to be written in a blood sugar diary so that the doctor or diabetes educator can see your results and advise on changes.
Why Does Blood Sugar Control Matter?
With gestational diabetes, it is all about the baby. If a mother has poorly-controlled gestational diabetes, then her blood sugar levels will be consistently high. This means the baby will be getting extra sugar across the placenta which can result in a baby growing larger than it otherwise would have. This may pose issues for delivery (such as an obstructed labour, shoulder dystocia and trauma to the perineum). It can also cause excess amniotic fluid (polyhydramnios), which may make it more uncomfortable for mum, but can also result in baby having an unstable lie and not getting engaged in the pelvis.
After delivery, there is a risk that the baby will develop LOW blood sugars. This is because the baby has been used to receiving the high sugars from mum, and has been compensating by producing excess insulin. When the baby is delivered, the supply from mum is instantly cut off, but the baby’s pancreas is still producing the extra insulin. Insulin works to push sugar from the blood into the tissues, and therefore may drop the baby’s blood sugar. The colostrum that the baby receives from breastfeeding may not be enough to keep the blood sugars up, and the baby may need to receive antenatally-expressed colostrum, formula, glucagon (an injection), glucose gel, or intravenous dextrose.
Diet
It is important to eat a wide variety of foods still, including carbohydrates, fats and proteins. Carbohydrate choices may need to be different in gestational diabetes. Foods that have a low Glycaemic Index (GI) will help slow the rise of blood sugar levels after eating. Carbohydrates that are brown or orange have a lower GI compared to white carbohydrates (ie brown rice/pasta, wholemeal/multigrain bread, sweet potato). It is also usually important to add in an evening snack. Fats and proteins also result in a more even blood sugar.
Exercise
Exercise does wonders for keeping blood sugar levels even. Just a walk around the block will help enormously. If there is a particular time of day that you are struggling to keep your sugars down, a walk at this time may be useful.
Medication
If, despite good dietary changes, the blood sugar levels are still too high, please do not feel like you have “failed”. It is simply a result of the interplay between your placenta and genetics. Medication may be needed to help manage your blood sugars. Often the tablet Metformin is used first. This tablet is taken between 1-3 times a day. It is usually well tolerated although can produce some gut upset.
If metformin doesn’t control the sugar levels, then insulin will need to be used. Insulin can be used before metformin – it usually depends on who is managing your pregnancy and which hospital you are having your baby at. An Obstetric Physician may be needed to oversee insulin regimes. Often, an injection of long-acting insulin at night is all that is needed. Needing insulin to manage blood sugar levels increases the chance of your baby requiring additional support postnatally, and delivery at an appropriate hospital may be necessary.
Changes in the Care During Your Pregnancy
Once diagnosed with gestational diabetes, you will need to see your doctor more frequently so they can check your blood sugar diary and make changes to your diet, exercise or medications. Due to the risk of baby being larger (or sometimes struggling to grow), extra ultrasounds will be needed.
Depending on the level of control of the diabetes, plans for induction of labour may be advised. If your blood sugar levels have been well controlled, and the baby is of normal size with no other complications, then we do not have to intervene until 6 days overdue. Induction from 38 weeks is advised if your blood sugars have been above target, the baby is large, there is excess fluid around baby, or other obstetric complications have occurred. If the baby is believed to be below 4 kg, a vaginal delivery can be planned for. If it is in excess of 4-4.5 kg, a discussion about an elective Caesarean Section should take place.
After delivery, the baby will need its blood sugar level tested at 1 and 4 hours of age. Generally, any medication needed during pregnancy can be ceased after delivery and no further finger prick blood sugar testing needs to happen. A repeat Oral Glucose Tolerance Test needs to be done at 6 weeks postnatal to make sure Type 2 Diabetes is not present.
Resources:
Morphology Ultrasound
The morphology scan, also known as the 20 week (2nd trimester) anatomy or anomaly scan, is recommended as part of routine antenatal care. The scan is ideally done at 19-21 weeks of pregnancy, when your baby’s growth and development can be seen more clearly.
This comprehensive ultrasound takes approximately 60 minutes and examines;
- The size of your baby.
- Baby’s anatomy, including a detailed assessment of the head, brain, face, lips, heart, stomach, lungs, abdominal wall, kidneys, bladder, spine, arms, legs, hands and feet.
- The position of your placenta in your uterus, ensuring it is not too close to the cervix.
- The length of your cervix, which can help in the assessment and prevention of preterm birth.
- The volume of fluid surrounding your baby.
- +/- your baby’s sex (if you would like to know).
- Maternal organs like kidneys and sometimes ovaries.
Most morphology scans show normal findings, but occasionally an abnormality is identified. If this occurs, your GP will discuss this with you and arrange appropriate counselling and follow up.
It is important to note that not all abnormalities can be detected by ultrasound. Some conditions may only become evident later in pregnancy or may not cause structural changes, such as cerebral palsy, metabolic conditions, some chromosomal abnormalities, or minor heart abnormalities.
Sometimes your baby’s position or movement can limit the sonographer’s view at the time of your ultrasound. In these circumstances, you may be asked to rebook for further assessment.
Morphology scans are usually performed transabdominally, but there are some circumstances where an internal/transvaginal ultrasound may be recommended to you. This involves your consent to insert a thin ultrasound probe into your vagina to get a better view of some structures, in particular your cervix and placental edge. A transvaginal scan is your choice, it is your decision whether you choose to consent or decline this aspect of the morphology scan. Both transabdominal and transvaginal ultrasounds are safe in pregnancy.
Options for First Trimester Screening
Attached below is a summary of optional screening tests in the first trimester for chromosomal trisomies in the fetus. As always, not screening is always an option. Choosing a screening test does not mean you need to progress to an invasive diagnostic test if it comes back at increased risk, and it certainly does not mean you need to progress to a termination of the pregnancy.
There is a specialist obstetric unit at the Women’s and Children’s Hospital that is very good at guiding families through all their options if they have an increased risk report. As always, the team at Adelaide Mums and Babies Clinic can explain things in more detail and help you make the right decision for your family.
Options for Pregnancy Care
We understand choosing the right care provider and place to birth your baby can be confusing and overwhelming – your midwife or GP can support you to choose the right option for you.
When deciding on your pregnancy care provider it is important to consider: location; cost (including level of insurance cover); pregnancy risk; levels of continuity of care; and whether your care provider’s philosophies align with your own.
We hope our summary below of the options within South Australia helps with your decision making.
Who can I see for my pregnancy care?
Public Hospital Care
Delivering in a Public Hospital would be the most commonly chosen option. If you have a Medicare Card, there are no fees to pay for visits to the hospital, nor for the delivery. There may be out of pocket costs for ultrasounds. If you choose to deliver in a Public Hospital, you will be zoned to a particular birthing hospital based on your post code.
Each public hospital offers different models of maternity care. Depending on the hospital and the risk level of your pregnancy, your care options may include:
- GP Shared Care
We delight in being able to provide care during this special time. All of our GPs are Obstetric Shared Care providers in South Australia and therefore are able to provide care during your pregnancy in conjunction with major birthing units.
Additionally, Dr Andrew provides intrapartum care at Mount Barker Hospital on a rostered basis. Dr Smith, Dr Andrew and Dr Gibbs hold Advanced Diplomas in Obstetrics and are able to manage more complex antenatal care.
Your birthing hospital will ask you to attend a triage or booking appointment around 14-20 weeks. Depending on your clinical needs, your GP will provide the majority of pregnancy care, but you will see the hospital for some of your pregnancy appointments (usually 20 weeks, 36 weeks and 40 weeks). During labour and/or birth, you will be cared for by the hospital’s midwifery and medical teams. After the birth of your baby, your GP would like to see you for a 2 and 6 week check.
This option provides excellent continuity of care for your pregnancy appointments and post-natal care (and beyond!).
There is no cost for your appointments at the hospital, nor for your labour/delivery and postnatal stay, but there will be out of pocket costs for your appointments with your GP.
- Midwifery-led antenatal clinic
Midwifery led antenatal clinics provide care to low risk women during pregnancy. If you attend the midwives clinic you will likely see a different midwife for most visits, and your visits will be at the hospital and there is no fee. A doctor will likely see you the first or second time you visit the Hospital and again later in your pregnancy, if needed. A different team of midwives will assist you during and after the birth of your baby.
- Doctor-led antenatal clinic
Obstetric antenatal clinics provide care for women at low and high risk of pregnancy complications. The doctor you see may change at each of your visits. A combination of midwifery and medical care is provided as needed and all of your visits will be at the hospital, with no out of pocket costs. A different team of doctors and midwives will assist you during and after the birth of your baby.
- Midwifery Group Practice (MGP) or Caseload Midwifery
MGP or caseload midwifery enables women to be cared for by the same midwife (primary midwife) supported by a small team of midwives throughout their pregnancy, during childbirth and in the first 6 weeks at home with a new baby. If you are interested in MGP, please let the midwife know during your first appointment at the hospital, as places are limited. Many of your pregnancy appointments will often be done at your home with no out of pocket costs. Flindes Medical Centre only allows low risk women to be cared for in this model; whereas Women’s and Children’s Hospital and the Lyell McEwin Hospital have all-risk models. All hospitals offer home birth to eligible women through this program. This model of care provides exceptional continuity of care for all of your pregnancy appointments, your labour and delivery, and 6 weeks of postnatal support. You will still need to find a GP for baby’s immunisations at 6 weeks and ongoing care into the future.
- Aboriginal Family Birthing Program
Some public hospitals offer Aboriginal women or women having an Aboriginal baby continuity of care with an Aboriginal Maternal Infant Care (AMIC) worker and a midwife/obstetrician in Aboriginal Family Birthing Programs.
Private Hospital Care
- Private Care with an Obstetrician
As a private patient, you will see your Obstetrician in their consulting rooms for your pregnancy care. Your Obstetrician, or sometimes another Obstetrician who works in the same practice, will attend the birth of your baby alongside the hospital’s midwifery team.
You will need a referral from your GP prior to seeing a private Obstetrician for care.
Not all private Obstetricians deliver at all private hospitals. The private hospitals that currently offer maternity services are Ashford, Burnside and Calvary North Adelaide. Each hospital lists the Obstetricians that deliver there (see below for links to their websites).
Some Obstetricians also offer deliveries at public hospitals.
You will need to have Top Hospital private health insurance to birth in a private hospital. You do not need Top Hospital Cover to deliver in a public hospital with a private Obstetrician, but you do need some level of Private Hospital Cover in most cases.
There will be out of pocket expenses for potentially all of your antenatal appointments, the planning and management fee half way through your pregnancy, and the excess for your hospital stay. There may also be fees to pay the Anaesthetist and the Paediatrician. Each Obstetrician will be able to provide you a fee schedule if you enquire.
Booking into the private hospital is usually overseen by your private Obstetrician who will provide you with the forms. Many hospitals have electronic forms you can complete.
Private Hospitals and Delivering Obstetricians:
Private Midwives
A privately practising midwife is an endorsed midwife who is self employed or employed within a private group practice. The majority of privately practicing midwives do not have admitting rights to South Australian hospitals, this means they are not able to be your care provider in a hospital setting and are only able to provide birthing services for women in their homes. The one exception is Sue Macfarlan who delivers at Lyell McEwin Hospital. There are costs associated with this model of care, although a Medicare Rebate can be claimed for antenatal and postnatal visits. This model of care offers continuity of care for pregnancy appointments and labour and delivery at home, as well as 6 weeks postnatal. If you are transferred to a hospital, your care will be taken over by the hospital team and your midwife can only be a support person.
Rural Birthing
There are many birthing hospitals in Rural and Regional South Australia, and each has their own way of managing antenatal care and labour and delivery. If you live rurally, it is best to discuss with your GP all your care options. Rural hospitals can only deliver low risk women, and all have a BMI cut off of 40 at delivery.
How do I book into a public birthing hospital?
If you have chosen to give birth at a public hospital, call the Pregnancy SA Referral Line on 1300 368 820 (available Monday to Friday, 9.00 am to 4.00 pm, excluding public holidays). You will be given an individual Reference Number and directed to the hospital you are zoned to. You then call the hospital and make a ‘Triage Appointment’ or a ‘Booking Appointment’. This is also the case for the 3 Regional Hospitals listed below.
Metropolitan Hospitals
- Flinders Medical Centre: 08 8204 5197
- Lyell McEwin Hospital: 08 8282 0255
- Women’s and Children’s Hospital: 08 8161 7592
Regional Hospitals
- Mount Barker: 08 8393 1715
- Gawler: 08 8521 2000
- Victor Harbor: 08 8552 0500
For a PDF version of this information, please click here.
Pregnancy Tips and Tricks
We’ve put together the answers to the most common questions we get asked by pregnant women. We hope you find this information useful!
What vitamins do I need?
Folate (0.5mg/day) should be taken from 1-3 months before conception, until 12 weeks of pregnancy. This is to reduce the risk of neural tube defects. Some women need to take MegaFol (5mg of folate). These women have a personal or family history of Neural Tube Defects (NTD), have had a previous pregnancy affected by NTD, have Type 1 Diabetes, are carrying twins, have a BMI >30 or are on medication for epilepsy.
Iodine (150 mcg/day) is recommended from before conception and throughout pregnancy. Iodine is important for thyroid function.
SAHMRI and SA Pathology offer testing for Omega 3 levels at the time of the first trimester screen and selectively recommending Omega 3 supplementation in women who are shown to be deficient; or ceasing additional supplementation if levels are high, in order to reduce the chance of preterm delivery. Please discuss this with your doctor or midwife for more information.
Aspirin 150mg taken at night, started in the first trimester or early second trimester, may be recommended by your doctor in some cases. Examples include: previous pre-eclampsia, pre-existing hypertension, a low Papp-A at first trimester screening, Type 1 or 2 diabetes, twins or higher-order pregnancies, pre-existing kidney disease, or autoimmune diseases such as lupus and antiphospholipid syndrome. If multiple of the following moderate-level risk factors are present, your doctor may also recommend aspirin. These include a BMI over 30, age over 35, first baby, or a family history of pre-eclampsia.
Additionally, if there is a risk of pre-eclampsia, calcium supplementation of 1200mg per day is needed, in addition to aspirin. Please consult with your care provider before commencing aspirin or calcium supplements.
Vitamin D universal supplementation of 400 IU per day is recommended for all pregnant women. Targeted testing for those at risk of Vitamin D deficiency is also recommended and if levels are low, 1000 IU per day will be needed.
What dietary changes do I need to make?
Pregnant women need to be aware of foods that are high risk for listeria, salmonella, mercury and vitamin A, and avoid these foods during their pregnancy. Examples include: soft cheeses, deli meats, unwashed fruits/vegetables, smoked salmon, sushi, uncooked egg (including real mayonnaise), fish high in mercury such as swordfish, soft serve ice-cream, paté and offal. The NSW Food Authority has good information on this. See www.foodauthority.nsw.gov.au.
An increase in nutrients is ideal in pregnancy. This means eating a well-balanced diet with plenty of different coloured vegetables; food rich in iron; calcium; protein and whole grains. You do not need to eat for two, nor increase your daily calorie intake. Just focus on eating a variety of nutritious foods.
Alcohol and smoking should be avoided at all stages in pregnancy. Please discuss with us if you are struggling to reduce or quit. We can support you.
Caffeine: small amounts are fine (1-2 caffeinated drinks per day), but excessive amounts can risk miscarriage and premature delivery.
What vaccinations are recommended in pregnancy?
The influenza immunisation is recommended to all pregnant women, at any time in their pregnancy. Pregnant women are at a higher risk of complications from the flu.
A whooping cough (pertussis) booster is recommended after 20 weeks, for all pregnant women. This is designed to significantly reduce the chance of your baby contracting, or getting seriously ill, from whooping cough before they have their own immunisations at 6 weeks. This is given during every pregnancy, regardless of when the woman had her most recent booster. Family members that will be in close contact with a baby before it is 2 months of age, are recommended to have a booster for whooping cough if they have not had one in the last 5 years. The government provides free immunisation to pregnant women, but not to family members. Your GP will be able to arrange how to immunise your family.
Covid-19 immunisation is not routinely recommended in pregnancy. However, if you are unvaccinated or have other medical conditions, this may be worth discussing with your GP or care provider.
A respiratory syncytial virus (RSV) vaccine is recommended for all pregnant women between 28 and 36 weeks. RSV is a leading cause of airway and lung disease in infants aged less than 12 months old. Receiving an RSV vaccine during pregnancy helps to protect your baby from serious illness and hospitilisation in their first year. The RSV vaccine is free for eligible women under the National Immunisation Program.
What screening tests are offered in pregnancy?
Blood Tests: many are requested at the start of pregnancy. The standard ones include: Full blood count, blood group and antibody testing, HIV/Hepatitis C/Hepatitis B/syphilis serology; Rubella immunity; iron levels; Omega-3 levels; and a urine test for a urinary tract infection. Sometimes, additional testing may be offered such as: thyroid function; chlamydia testing; cervical screening if due; vitamin D levels; and immunity to other viruses.
Additional bloods are requested at 28 weeks. These include screening for gestational diabetes with an OGTT, full blood count, blood group antibodies and iron levels. Additional blood tests may be requested if clinically indicated.
Gestational diabetes screening may also happen between 12-16 weeks if women have risk factors for having early-onset gestational diabetes.
First Trimester Screening: is offered to assess the chance the fetus has a chromosomal trisomy (T21 – Down’s Syndrome; T18 – Edward’s Syndrome; +/- T13- Patau’s Syndrome, +/- 22q11.2 – DiGeorge Syndrome). There are 2 options for this.
1) First Trimester Screen (FTS) (Medicare rebatable): This involves a blood test from 9 weeks to assess for Papp-A and bHCG levels; and an ultrasound at 12 weeks looking for the nuchal translucency (the thickness at the back of baby’s neck). These results, along with age, ethnicity, weight, smoking status etc are put into a calculator and a risk report is generated. Levels that are less risky than 1:250 are classified as “not at increased risk” and levels more risky are classified as “at increased risk”. Women who have a risk result that is MORE risky than their age-related risk, may also be classified as “at increased risk”. These results need to be discussed in a nuanced fashion as the level of acceptable risk is up to the woman and her family.
2) Non-Invasive Prenatal Testing (NIPT) (Non-Medicare rebatable): this is a blood test done from 10 weeks, and compares the fetal DNA in the mother’s blood to her own DNA to try and detect abnormalities. It can also detect sex-linked chromosomal abnormalities and the sex of the fetus. The cost varies, but is around $530 and done at various pathology labs. Common names include the Nest test, the Harmony test, or Generations.
Regardless of the result of this test, all women also need an early anatomy scan at 12-13 weeks as the NIPT does not rule out structural abnormalities of the fetus.
Women that have a high risk First Trimester Screen, may also opt for a NIPT before undergoing an invasive diagnostic test. The NIPT result will always trump the result of the First Trimester Screen, and may avoid the need for an invasive diagnostic test.
Both the First Trimester Screen and the NIPT are considered screening tests. This means – any “at risk” result will need diagnosis by an invasive test that directly tests the baby’s DNA. The two options are a CVS (sample of the placenta from 10-13 weeks) or an amniocentesis (sample of the amniotic fluid done from 15-20 weeks). Both of these tests carry a risk of miscarriage and appropriate counselling is done prior to performing these tests.
Genetic Carrier Screening (medicare rebatable for fragile X, spinal muscular atrophy and cystic fibrosis): we are all carriers of around 2 severe autosomal recessive conditions. This test is only performed ONCE in a woman’s life, and is actually recommended prior to conception but can be done early in pregnancy. The chance a woman is a carrier of an autosomal recessive condition is 1:20. If she is a carrier, her partner is tested to see if he is also a carrier. The chance of both parents having the same autosomal recessive gene for one of these 3 conditions is 1:240. You need BOTH parents to be carriers for there to be a chance of their baby inheriting the particular condition. Other more comprehensive genetic carrier screening can be done for over 400 autosomal recessive conditions. The cost of this ranges from $550 to $700 for the woman; or $750 to $1200 for the couple.
Can I exercise during pregnancy?
Exercise is generally safe during pregnancy, particularly if you have been doing the same activity before you were pregnant. Always listen to your body and stop or rest if you experience any pain. It is important to not overheat, so exercise in a well-ventilated area and keep hydrated.
Pregnancy pilates or yoga classes are a firm favourite with many women. They help improve core and pelvic floor strength and can help with many musculoskeletal issues in pregnancy.
I have cats – I’ve heard this is an issue?
The problem with cats and pregnancy is due to the risk of getting toxoplasmosis from their faeces. If you’re going to change their kitty litter, wear gloves, wash hands, or better still, delegate to someone else!
Toxoplasmosis is also present in soil, so be careful when gardening too. The symptoms of toxoplasmosis are very similar to the flu.
Can I have sex?
Generally, there is no issue with having sex while pregnant. Towards the later stages of pregnancy you may have to be creative with positions that are comfortable.
There are a few obstetric conditions where sex is best avoided. This is in the case of placenta praevia (where the placenta is low lying and covers the cervix); with recurrent threatened preterm labour; a short cervix; or ruptured membranes/amniotic fluid leak.
What medications should I avoid?
Your doctor should inform you if any prescribed medications you are on are unsafe in pregnancy. The vast majority are acceptable to continue.
The main over-the-counter medication that is best avoided while pregnant is ibuprofen and other anti-inflammatories.
The Women’s and Children’s Pharmacists are the best resource for what is safe to take during pregnancy and breastfeeding. You can contact them Monday to Friday 9am-5pm on (08) 8161 7555.
How do I manage the common pregnancy symptoms?
Reflux
This is a very common problem in pregnancy. You can try eating small meals, avoiding caffeine and chocolate, or trying over-the-counter options like Mylanta, Gaviscon and Quick-eze. Stronger acid-suppression tablets (proton-pump inhibitors) are available on script and are safe in pregnancy.
Nausea and Vomiting
Experienced by the vast majority of women in early pregnancy, luckily most cases are mild and transient. For those that are suffering you can try things like: eating small amounts often; eating before getting out of bed; drinking semi-flat fizzy drinks; ginger ale/biscuits/tablets; eat plain and easy to prepare meals; and B6 tablets. The next step is Restavit (a sedating antihistamine, available over the counter). Try ¼-½ tab at night initially and increasing the dose as needed and tolerated. Beyond this, prescriptions are needed. Options include Maxolon and Ondansetron, or a combination of these. Ondansetron can cause constipation so you may need to start a laxative.
Constipation
This can hit early and it’s because of the high progesterone in pregnancy slowing down gut transit time. Later in pregnancy, it is because of the large uterus further slowing things down. It is important to drink lots of water, try and stay active, and increase fibre in the diet. If this doesn’t work, try adding 2 Coloxyl tablets at night and increasing to twice a day. Coloxyl is a softener and won’t make the bowel lazy. The next step is adding Movicol sachets and/or Lactulose syrup. If this isn’t working, touch base with your doctor to discuss other options.
Fatigue
This is usually worse in the first trimester and abates over time. If it is persistent, getting your iron levels checked is a must. Unfortunately it is also common to experience insomnia while pregnant, which doesn’t help the situation!
Leg Cramps
These seem to be more common in pregnancy and the cause is poorly understood. Low iron levels can sometimes be to blame – so make sure yours are checked. Magnesium tablets can be helpful. As can keeping hydrated, stretching before bed, and Epsom salt baths.
Ankle Swelling
As long as it is mild, this is usually just a common pregnancy complaint. Try keeping your legs moving, not standing for long periods and wearing compression socks/tights. If your swelling suddenly increases, or involves your fingers or face, it is important you see your doctor or midwife ASAP to get your blood pressure and urine protein levels checked. This can be a sign of pre-eclampsia.
Fainting
For some women, the physiological drop in blood pressure can cause all sorts of trouble with fainting or dizzy spells. Simple measures include: staying hydrated, eating plenty of snacks, standing up slowly, not standing for prolonged periods, wearing TEDs stockings or other compression tights, and lying on your side rather than your back.
Back Pain
A very common pregnancy complaint! Some will just get the odd niggle while others will be plagued with continuous discomfort and/or symptoms of pelvic instability or pubic symphysis pain (SPD). A women’s health physio is the best person to manage this for you. Supporting your belly with a tubi-grip can be useful, as well as maintaining fitness and flexibility. Pelvic instability and SPD can be managed with a brace or SRC shorts/leggings if needed.
Sleeping positions
From 20 weeks of pregnancy, your uterus is usually up to your belly button. This is where the inferior vena cava (the main vein bringing blood back to your heart) starts. If you lie on your back when you are over 20 weeks, there is a chance this vein will get compressed, causing a decrease in cardiac output. This can result in feeling faint, breathless, and also reduce blood flow to the placenta which can stress your baby. It is advised to sleep on your left side. At a minimum, placing a pillow or wedge under your right hip should displace the uterus off your vena cava.
Stretch marks
Despite what is often claimed, not much can be done to prevent stretch marks. It is usually up to your genetic predisposition as to how your skin will tolerate the stretch during pregnancy. Keeping the skin well moisturised is your best defence, as well as not gaining excessive weight.
Is it safe to travel in pregnancy?
Most airlines will let you travel up to, and even beyond, 36 weeks within Australia if you have a singleton pregnancy. International travel has earlier restrictions. The airlines will need a letter from your doctor once you are past 28 weeks confirming you have an uncomplicated pregnancy. Letters generally need to be completed no more than 10 days before travel. All airlines publish their requirements for travelling when pregnant on their website. It is best to check with your specific airline before booking.
The safest time to travel is in your second trimester. It is best to avoid developing countries during your pregnancy due to the increased risk of infections and poor food and water quality. The most important aspect of travelling while pregnant is travel insurance. It can be very hard to find insurance for yourself, and even harder for a baby if it happens to come early while overseas. The costs of a hospital stay and NICU bed for your baby can be enormously expensive, especially in the USA where bills over AUD$500,000 are not unheard of.
Malaria is prevalent in some areas and is transmitted via mosquitoes. Malaria is associated with severe anaemia, miscarriage, stillbirth, fetal growth restriction and preterm birth. If you cannot avoid travelling to an area with high rates of Malaria, consider minimising outdoor activities between dusk and dawn, wear long sleeved clothing and sleep under mosquito nets. If you are travelling to an area with highly resistant malaria strains, you may require oral medication to minimise the risk of infection. Please discuss any concerns with your doctor.
Zika virus is also transmitted by mosquitoes. Pregnant women should avoid travelling to Zika virus affected areas. Zika virus can cause; rare congenital development malformations in babies born to mothers exposed to Zika virus and rare neurological conditions such as Guillain-Barre Syndrome.
Prevention of DVT (deep vein thrombosis) is important when travelling long distances by plane or car. Make sure you move your ankles and pump your calf muscles often during the journey. Keeping hydrated is also important (although may increase the swelling in your ankles). Avoid alcohol and caffeine. You can consider using travel socks or TED stockings. And most importantly – take your Pregnancy Hand Held Record with you!
Reproductive Genetic Carrier Screening
The Royal Australian College of Obstetricians and Gynaecologists (RANZOCG) is now recommending that information on carrier screening should be offered to all women planning a pregnancy or in the first trimester of pregnancy. This is not the same as First Trimester Screening (FTS) or Non Invasive Prenatal Testing (NIPT) which is offered to test a fetus for Trisomy 21 (Down Syndrome), Trisomy 18 and in some cases additional chromosomal anomalies. These last two tests are offered in every pregnancy as they are specific for the individual fetus.
Genetic Carrier Screening is a genetic test for an adult, typically done by taking a blood or saliva sample, to determine if a person carries a recessive copy of a gene for specific genetic conditions. The genetic conditions tested for are – Spinal Muscular Atrophy (SMA), Cystic Fibrosis (CF) and Fragile X syndrome (FXS). They are some of the most common inherited recessive conditions in our population and have serious health consequences. A person may be a carrier without knowing and most do not have any family history of these conditions. In order for a person to have this condition, they need to inherit a recessive gene from both parents.
To red more on this topic, including specifications of Spinal Muscular Atrophy (SMA), Cystic Fibrosis (CF) and Fragile X syndrome (FXS), please click here to view the PDF version.
Antenatal Education
Antenatal Classes
We love providing antenatal education to the parents and families of Adelaide. We have multiple classes available to help you feel prepared and supported in caring for your newborn.
Tell me more!
So many women we see with breastfeeding issues wish they had known all this before they had a baby. Although breastfeeding is natural, it can be one of the most difficult things you will ever do.
Topics include…
- Antenatal colostrum expression and storage
- Anatomy and physiology of breastmilk production
- Extraction of breast milk
- The first few days (the hospital stay)
- After your milk “comes in”
- Engorgement and low milk supply
- Being separated from your baby
- Paced bottle feeding
- Gestalt Breastfeeding – fit and hold (an evidence-based approach to significantly reduce nipple pain, improve milk transfer and decrease fussing at the breast).
- Q&A session that answers individual questions and concerns.
How do I book?
Bookings can be made online through our HotDoc page or by calling the clinic.
Online bookings can only publish class dates 3 months in advance. If you see a scheduled time that you would like to attend, please contact the clinic and we can book you in.
See more information and upcoming class availability here!
Tell me more!
Parents often receive conflicting advice when bringing their newborn home. This class will empower you to raise your baby in a cued-care approach and have confidence in your parenting skills.
Topics include…
- Parenting values clarification
- Infant sleep
- Infant settling – ” The Two Tools”
- Feeding (both breast and bottle feeding)
- Parental mental health and wellbeing (managing difficult thoughts and feelings in the perinatal space)
How do I book?
Bookings can be made online through our HotDoc page or by calling the clinic.
Online bookings can only publish class dates 3 months in advance. If you see a scheduled time that you would like to attend, please contact the clinic and we can book you in.
Bringing Baby Home ONLINE!
“Helping you navigate the first few months with your baby…”
We are very excited to share our exceedingly popular course, Bringing Baby Home, as an online product. Parents that attend our in-person class rave about it. Now, no matter where you are in the world, you can experience the same education. We have expanded on our in-person course by providing more detail around mental health support, feeding, and infant sleep and settling tips.
This course is perfect for any parent-to-be, including those having a subsequent child. The approach we take is quite different to what is available from most other infant-care resources. However, what we focus on is evidence based and designed to set realistic expectations of early parenthood. We want you to enjoy this transition, while fully acknowledging that all transitions bring with it mixed emotions and feelings of uncertainty. We promote experimentation so that each family can find what works best for them.
We highly recommend starting this course during your pregnancy, but there are so many topics that are relevant throughout the first year of life. Gift certificates are available for loved ones as the perfect baby shower gift.
Our online course Bringing Baby Home is valued at $249 but is currently reduced to just $99. 6 months of access allows you plenty of time to get your head around things while pregnant, as well as looking back over the relevant topics during your baby’s fourth trimester.
LEARN MORE - CLICK HERE
1:1 Antenatal Education Appointments
Do you feel like you have no idea what to do when you bring baby home? You may want to get yourself prepared for parenthood while you are pregnant, and arm yourself with evidence-based information on baby-caring.
Many of our GPs offer one-hour long consultations focused on educating you about feeds, sleep and sensory nourishment to make the first year of baby’s life a thoroughly enjoyable experience. Babies can be unsettled in the first 3 months, but there are many strategies you can use to help keep baby dialled down. We offer a unique approach to caring for your baby – one that is relaxed, flexible, and based in cued-care. Many parents who use a similar style report lower levels of postnatal anxiety and depression. The best time to book this appointment is in the third trimester of pregnancy.
We also offer Antenatal Breastfeeding Education 1:1 consults for those mothers that wish to get the best start for their breastfeeding journey, or mothers whose previous journey was troublesome. We will take the time to educate you on the Gestalt Breastfeeding Program, write a breastfeeding plan for you to take to the hospital, as well as educate about common breastfeeding problems. We can also provide education on antenatal expression of colostrum if you wish to take a supply with you to the hospital. This consult is best done in the third trimester, in an hour-long appointment.
Antenatal Reading
The Discontented Little Baby Book – By Dr Pamela Douglas
This is the only book you need to read to prepare for looking after a baby.
The Discontented Little Baby Book is available for purchase at our Rose Park and Ashford clinics and is written by Dr Pamela Douglas, founder of Neuroprotective Developmental Care (NDC) or the “Possums Program”. This book gives you a revolutionary new approach to caring for your baby’s needs from a respected Australian GP.
You will learn practical and evidence-based strategies for helping you and your baby get more in sync – which also protects your sleep. Dr Pamela Douglas offers a path that protects your baby’s brain development so that your little one can reach their full potential. Amidst life’s extraordinary challenges, Dr Pamela Douglas shares practical strategies not only for cherishing your baby but also for nurturing your own rest and vitality.
With real-life stories from other parents, advice on dealing with feelings of anxiety and depression, and answers to your questions about sleep, development, reflux, allergies and tongue-tie, The Discontented Little Baby Book is a compassionate revolution in baby care.

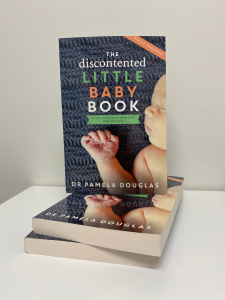
Price: $30.00
Appointment Booking Reminder
To book an appointment, please:
- Call reception OR
- Book online via our website or booking app (HotDoc)
- If you’ve booked online but feel your issue is more urgent, please call reception directly — we may have reserved urgent appointments available.
**Please note:**
Appointments cannot be made by emailing the clinic, doctors, or nurses. This ensures all bookings are handled promptly and appropriately.
Thank you for your understanding and helping us provide the best care possible.



